Labwork
Prenatal lab-work is scheduled at your first official appointment (the first appointment after your free consult). One blood draw is required and the blood is sent to either LabCorp or Quest Diagnostics for evaluation.
At 18-21 weeks we schedule your sonogram. This is the best time to have the test because all of the organs are formed and it is the best time (for you) to see the sex of the baby. Although that is the biggest reason moms and dads want to have a sonogram, your midwife is looking at different things. As an out-of-hospital healthcare provider, we want to make sure the baby is well formed, that the placenta looks good and know where it is located, and take a look at the heart and lungs.
At 28 weeks of pregnancy, we perform routine testing of your blood sugar (see the 28 week visit section for more details) and hemoglobin (checking for anemia), and offer the HbsAg test again. If you are an Rh negative mommie, we also test your Rh status at this point. Rh negative moms have to have this additional blood draw.
At 36 weeks, this is one last time to check your hemoglobin, test for Group B Strep, Gonorrhea, Chlamydia and offer the HbsAg test again, as well as the antibody screen again if mom is Rh negative.
Tests routinely performed in the first trimester:
Complete Blood Count (CBC)
Blood Type and Rh Factor
Hemoglobin and Hematacrit
Sexually Transmitted Disease Screen (RPR)
Hepatitis B Surface Antigen Test (HBsAg)
Rubella Status
Urinalysis/Urine Culture
Optional Lab Tests Offered:
Cystic Fibrosis Carrier Screening
Maternal Serum Alpha Fetal Protein Test (MSAFP)
Chorionic Villus Sampling / Amniocentesis
Ultrasound or Sonography
HIV Screening
Gonorrhea & Chlamydia Cultures
28 Weeks Gestation
You’re more than half way through your pregnancy!!! Between 24 and 28 weeks gestation, in addition to the routine prenatal visit procedures, we will also review fetal kick counts and belly mapping. A few lab tests will be performed during this visit and after this appointment we will start seeing you for prenatal visits every two weeks until you reach 36 weeks.
When you arrive for your appointment, you will be given Fresh Test to drink, which is a diagnostic 50g glucose beverage. We will perform a blood draw and obtain a blood sample to measure two different lab results.
One is the glucose screening (blood sugar) testing for gestational diabetes. The results of this test should be no higher than 135. If this screening is high, then a diagnostic 3-hour glucose test will be performed.
The other is to test your hemoglobin (iron level). We measure your hemoglobin to make sure that you are not anemic. At this point of pregnancy, your blood volume has increased by as much as 50 percent, as it assists carrying oxygen throughout your body and to the baby. This is called hemodilution. At this stage, although your blood volume has increased, it is just as described–diluted, and not as rich and thick as it will be toward the end of pregnancy. If your hemoglobin is below 10.5 gm/dl, we will review dietary changes and recommend a suppliment to increase your hemoglobin. It will then be rechecked in two weeks. The range we like to see hemoglobin (also called hgb) is at around 12 gm/dl.
For our Rh negative mommies, we will also screen you for antibodies and provide a rhogam shot if needed. We will discuss this more at your visit.
Fetal Kick Counts
You have probably noticed that your baby moves a lot after 24 weeks. Fetal movement is a good indicator of the baby’s well being. It is a great idea to do daily kick counts beginning around 28 weeks. Kick counts are done as follows:
Pick out a time in the evening after supper when you can lay down and pay attention to your baby. Note the time. Begin counting the baby’s movements. At the tenth movement, note the time again. It generally takes less than one hour to get 10 movements. If you've reached an hour and have not gotten 10 movements call and speak to a midwife. Noticing when your baby moves is a good indicator for what they'll do on the outside.
Non-Stress Test
A non-stress test involves monitoring a babies heart rate along with any contractions you may be having. We expect to see the heart rate accelerate twice in a 20 min period. This assures us the placenta is functioning and baby is oxygenated well. We are able to do this at the center and not the hospital.
If you have reached 41 weeks or have special health problems, we might have you do a special test called a “non-stress test” (NST). This involves being placed on the fetal monitor for approximately 20-30 minutes. The baby’s heart rate will be monitored. Just as your heart speeds up when you exercise, so should your baby’s. A normal NST reassures us that the baby will probably remain healthy for the next three to four days.
Preparing Family
The birth of your child is a very intimate experience. As midwives we protect this space both physically and emotionally. We encourage anyone who wants to be present at the birth to also attend childbirth classes and prenatal visits. Any family members who are not comfortable with child birth or out-of-hospital births are encouraged to wait till after the birth to come see the family. We encourage the couple to assign jobs to anyone attending the birth so that the focus is on the mother and the intention of a safe and joyous birth.
Other Family Members
The birth of your child is a very intimate experience. As midwives we protect this space both physically and emotionally. We encourage anyone who wants to be present at the birth to also attend childbirth classes and prenatal visits. Any family members who are not comfortable with child birth or out-of-hospital births are encouraged to wait till after the birth to come see the family. We encourage the couple to assign jobs to anyone attending the birth so that the focus is on the mother and the intention of a safe and joyous birth.
Safety Concerns/Transfers
The birth of your child is a very intimate experience. As midwives we protect this space both physically and emotionally. We encourage anyone who wants to be present at the birth to also attend childbirth classes and prenatal visits. Any family members who are not comfortable with child birth or out-of-hospital births are encouraged to wait till after the birth to come see the family. We encourage the couple to assign jobs to anyone attending the birth so that the focus is on the mother and the intention of a safe and joyous birth.
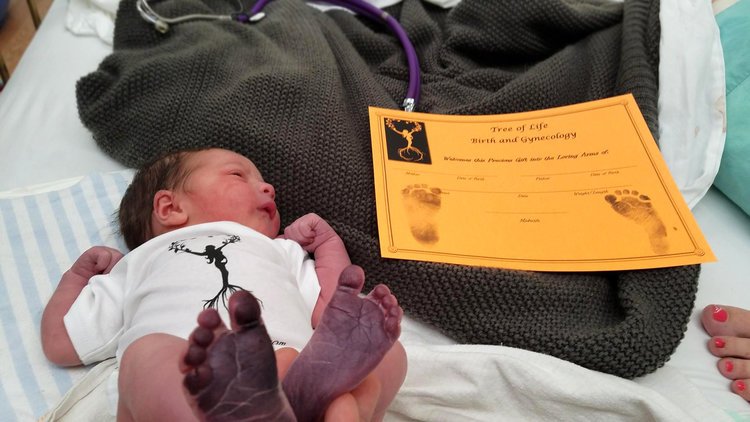
After the Birth
The first hour after the birth is the most critical and precious. Allowing the cord to complete pulsing and maintaining skin to skin is optimal in assisting the newborn in transitioning to extra uterine life. We assist with breastfeeding and encourage latch in the first hour. Maternal and infant vitals are monitored regularly per protocol. We perform a complete newborn exam, offer newborn medications, birth certificate and social security filing. Mom and baby are monitored for a minimum of two hours after the birth. We encourage a hearty meal with protein and provide postpartum teas. Mom and baby will both be tired, so letting them rest the first day is advisable. The most important place for the baby is with momma! Prior to discharge the staff will review instruction on vitals signs to be done every 4 hours in first 24hrs then daily. You will report in to a midwife daily to review vitals, well-being, and have gentle reminders of self care, normal postpartum symptoms, and any support you may need. The first three months with your newborn are referred to the Fourth Trimester. This is the time of recovery, bonding, and nurturing both the baby and the family.We recommend preserving this time with intimacy and rest. Avoiding to many visitors in a day, outings like shopping for the first month, and performing self-care activities like sitz baths, massages, regular naps, and postnatal yoga.